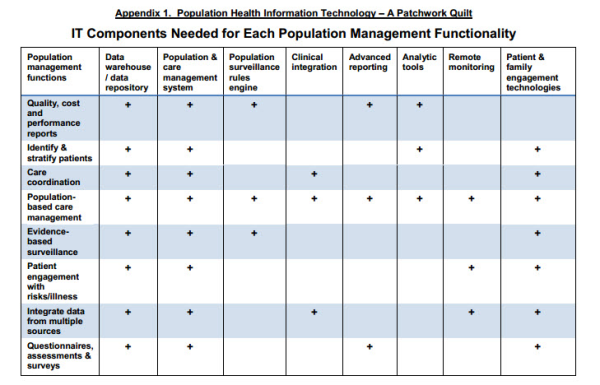
Population Health IT for ACOs: A Patchwork Quilt
by Ron Parton, MD, MPH, Chief Medical Officer of Symphony Corporation
The new ACO rule has big implications for information technology. In the final rule
on accountable care organizations (ACOs), CMS has included 33 measures that
report overall performance while allowing providers options to share in any
savings. Because the new ACO rule will no doubt steer payors and providers to
improve quality and reduce costs, the need for population health information technology
to support ACOs has dramatically increased.
Current reporting technology and electronic health records (EHRs) may be able to
provide basic reporting on the measures, but they are woefully inadequate at meeting
the ACO requirements for improving care, enhancing the patient experience and
reducing costs. New population and care management systems will be required to
support primary care medical home models, care coordination, case management, and
transitions of care. Advanced health care delivery will require the adoption of new
information systems and tools that:
• Provide rapid, flexible and continuous performance reporting
• Promote the proactive identification and management of the “highest risk” patients
• Accurately attribute patients to physicians and care teams
• Allow care teams to coordinate care across the entire continuum and
systematically manage multiple chronic illnesses
• Integrate information and work flows across population & care management
systems, EHRs, care teams, providers, community resources, and health
information exchanges (HIEs)
• Support “real time” decision making and population surveillance using evidence-based guidelines
• Engage, educate and support patients in self-care, prescription drug adherence, lifestyle improvement and prevention
• Aggregate and manage data from multiple disparate data sources (clinical, administrative & financial) with a reliable master patient index functionality
An array of technologies and information tools to piece together: A patchwork quilt
Integrated delivery systems such as Kaiser Permanente, Geisinger and Group Health Cooperative have incorporated population health information technologies to varying degrees to improve quality, reduce costs and enhance patient experience. These leading organizations found their EHRs insufficient for population health management. Since their electronic health records lacked this functionality, they ultimately developed and/or bought, and then pieced together their data, systems, tools and reports. In fact, these systems have spent a considerable amount of time and money on creating these tools themselves. These collections of support tools, registries, and systems are far from perfect, but have allowed these organizations to accomplish impressive results that have set them apart as national leaders in managing quality and cost. Organizations of physicians and hospitals that are striving to create ACOs can build on the experience of these integrated systems to improve their performance under healthcare reform. Building on top of an EHR, the following components create a population health IT system:
Data warehouse/data repository – Integrating multiple data sources including ambulatory and inpatient EHRs, labs, scheduling, billing, health information exchanges (HIEs), insurance claims, remote monitoring, patient selfreports, research, demographic, administrative and financial data
In general, the data warehouses that are included with EHRs are not designed for integrating financial, clinical, research and administrative data from multiple external sources or for use in tracking health care interventions and outcomes for populations. To improve and report on performance, an ACO will need to create a data warehouse and/or repository to store all available data on its patients and services and make these data available across the enterprise to support the population and care management initiatives.
Population health and care management system – Including an enterprise multi-disease registry with measures and reporting; work flow support & tools for case management and health coaching; care team performance tracking with an embedded rules engines to support follow-up tasks and reminders; creation and sharing of care plans that include longitudinal care views of goals and progress.
Chronic illness registry tools typically have been developed for single diseases and have produced lists of patients that need follow-up or have “care gaps”, but do not include case management tools or health coaching functionality to manage and/or document the work in coordinating care and assisting patients with their illnesses. These tools help to facilitate identification and can report the results, but they do not manage the workflow across multiple diseases or support case management/health-coaching. New population health and care management systems are now available that are multidisease and can help care teams with role-based task management, care coordination, prescription drug adherence, patient letters and reminders, life style tracking to goals, and comprehensive clinical and financial performance reporting. These population health and care management systems are complementary to and can integrate with EHRs. They are designed to be flexible and accommodate different work flows across the care teams and also allow for the inevitable changes in measures, definitions and guidelines that will occur from time to time with medical advances.
Population surveillance rules engine – To monitor care process and outcomes using evidence-based guidelines, with links to both a population and care management system and the EHR
Most EHRs will facilitate reminders that “pop up” during a patient encounter to flag the need for routine preventive screenings, immunizations, lab tests and care gaps, but they are not very flexible and do not connect to a follow-up tracking system that facilitates role-based work flow for the care team. Since EHRs are visit-based, they generally don’t trigger actions between encounters, don’t allow flexible workflows for follow-up across the care teams, and don’t document interventions or communication attempts. Evidence-based rules engines that exist outside of the EHR can support population management by the care teams for actions that are triggered, often avoiding the expense of a face-to-face visit with the practitioner. There are population health and care management systems that incorporate evidence-based rules engines for population surveillance and support care teams in closing the care gaps that are identified.
Clinical integration of systems - Integrates population health IT with
EHR functionality and work flow
While much of the routine population health and care management work can occur outside of the typical physician encounter, freeing up physicians to concentrate on the more urgent issues, difficult medical problems and complex patients, the complete set of information about each patient must still be stored in the EHR. This requires that new information generated in a population and care managements system be fed back to the EHR, so it is available at the point of care for decision-making and follow-up. In addition, there may be actions that are triggered in the population and care management system such as scheduling a lab appointment, a change in a prescription drug and/or a follow-up physician appointment that can be executed in the EHR. The work flow between the EHR and the population and care management system must be optimally integrated to help assure efficiency and access to the data. Over time, some of the population health functionality that isn’t available now may be incorporated in the EHR itself. However, EHRs are usually structured around encounters rather than populations, care teams, or non-encounterbased workflows. This may ultimately limit the capacity of most current EHRs to incorporate population health IT functionality.
Advanced reporting - Tracking financial, administrative and clinical performance
Decision making to support improved quality and reduced cost requires a full set of internal financial, administrative and clinical performance reports that measure their own performance against benchmarks as well as a full set of external reports for pay-for-performance programs and reporting to third parties including HEDIS, PQRS, ACO measures and statewide quality collaboratives.
Analytic tools – Focused on predictive modeling, episode grouping, severity & case mix adjustments
Predictive modeling tools (i.e. Johns Hopkins ACGs or Medicare’s HCCs) support proactive identification and stratification of the highest risk patients for potential referral to complex case management. A parallel methodology is also needed to measure cost and utilization with case mix adjustment, typically through episode groupers (i.e. OptumInsight’s Episode Treatment Groups or Thomson Reuter’s – Medical Episode Groups).
Remote monitoring technologies – Home-monitoring that interfaces with care management and EHRs
High-risk patients with certain chronic illnesses such as congestive heart failure, diabetes, hypertension and chronic obstructive pulmonary disease may benefit from utilizing home-monitoring devices that allow them to track their own illnesses and work interactively with a case manager and/or health coach that can also follow and track their outcomes in “real time.” This information can be sent back to both the population and care managemen systems and the EHRs.
Patient and family engagement technologies – Including web-based portals linked to personal health records; life style tracking tools; handheld technologies for education, tracking, reminders and interactive learning; webvideo technologies for virtual provider visits, health coaching and case management; and interactive assessments, questionnaires and connectivity to measure patient outcomes and provide feedback on patient experience
Patients are now being provided access to their own medical record information and encouraged to learn more about and manage their own health risk factors and chronic illnesses. Mobile and tablet technologies, web-based patient portals and web-video technologies are allowing patients to have better access to their care teams, medical knowledge and tools that help them to improve their lifestyles and achieve better results in managing their illnesses. These can be linked to both their population and care management tools and their EHRs. Patient experience questionnaires, interactive assessments for depression screening, assessment of activities of daily living, pain management follow-up, etc. can be administered using email, patient portals and/or handheld technologies. This information can be stored and tracked in the data warehouse and the EHR as needed. Families are using some of the same technologies for social engagement and monitoring.
Population Health Information Technology is Complex to Implement but Critical for ACO Performance
All the pioneering organizations participating in the Medicare Physician Group Practice demonstration, such as Marshfield Clinic, have significantly redesigned care workflows and introduced population health information technology that makes clinical data more readily available to the practitioners and care teams, including additional “add on” disease registries or embedded tools within their EHRs.
It may be disappointing that after having spent significant amounts of time, effort and money to implement electronic medical records across your own organizations, there is more work ahead in assimilating a complete set of population health information technologies to become a successful ACO. The consolation is that none of these pioneering organizations have used all of the population health and care management tools that are now available and yet most of
them accomplished positive results.
One of the keys going forward will be to prioritize the functions that are most likely to achieve results and implement those first. See the Appendix below for a matrix of Population Health IT and functionalities:
Dr. Ron Parton is Chief Medical Officer of Symphony Corporation, a global technology solutions provider based in Madison, WI. He may be reached at ron.parton@symphonycorp.com

Accountable Care News is a publication of Health Policy Publishing, LLC.





Your Comments :