When California launched its Self-Determination Program in 2019, most disability advocates didn't bat an eye at the name. But if you work in this space across multiple states, you've probably noticed the split: California calls it self-determination. Nearly everyone else calls it self-direction.
Is this just California being California? A big state doing its own thing in parallel while the rest of the country moved forward together?
Not quite. The terminology gap reveals something more interesting: two different philosophical entry points that led to the same destination. And understanding the distinction matters—not just for historical curiosity, but for how we build technology, write spending plans, and talk to families about what these programs actually promise.
The Self-Direction Story: Born in Medicaid Operations
Most states landed on "self-direction" because the term emerged organically from federal Medicaid policy discussions in the 1990s and early 2000s.
The Centers for Medicare & Medicaid Services (CMS) began talking about self-directed services as a service delivery model. The framework was operational and practical. It answered administrative questions:
- Who has the authority to hire and fire workers?
- Who approves timesheets and manages budgets?
- Who bears employer responsibilities under labor law?
- How do we maintain accountability while giving families control?
The emphasis was on direction—literally, who's steering the vehicle of service delivery. States adopted the language because it fit cleanly into Home and Community-Based Services (HCBS) waiver applications. It satisfied CMS requirements. It worked.
There's nothing wrong with this framing. It's precise, implementable, and crucially, it gave families real power over their supports. Self-direction transformed Medicaid from "we'll send you whoever's available on Tuesday" to "you choose who shows up, when they show up, and what they help you with."
That's revolutionary, even if the language sounds bureaucratic.
The Self-Determination Story: Born in Disability Rights
California came at the same destination from a completely different direction.
The state's Self-Determination Program didn't grow out of Medicaid operations meetings. It emerged from decades of disability rights advocacy and a deep cultural commitment to person-centered planning within California's Department of Developmental Services (DDS).
The philosophical backbone came from:
- The independent living movement of the 1970s and 80s
- Ed Roberts and the Berkeley disability rights community
- A long tradition inside California DDS of framing disability supports as civil rights, not charitable benefits
- Person-centered planning methodologies that put the individual, not the system, at the center
Self-determination answers a fundamentally different question than self-direction. It's not asking "who manages the supports?" It's asking: "Who decides what a good life looks like?"
That's a much bigger claim. It's about agency over your entire life, not just administrative control over your service budget. It positions the program as a tool for self-actualization, not just efficient service delivery.
California wasn't trying to be different. They were being intentional about the values they wanted to center.
Self-Directed Medicaid Home Care Services in 2026
To see how these models show up across different waivers and states, check out our overview of self-directed Medicaid home care services in 2026, which connects the terminology to real program designs.
Two Paths, Same Promise
This wasn't California rebelling against federal norms or reinventing the wheel out of stubborn independence. It was parallel evolution driven by different starting philosophies:
Most states: Medicaid-led, operations-first thinking → self-direction
California (and others influenced by rights-based models): Disability-led, values-first thinking → self-determination
Both paths led to remarkably similar programmatic structures:
- Participant-directed budgets
- Individual service plans
- Employer authority over workers
- Financial Management Services (FMS) support
- Person-centered planning requirements
Same mechanical house. Different front doors.
Think of it this way:
| Term |
Primary Emphasis |
Core Question |
| Self-Direction |
Control of service delivery |
"Who manages the supports?" |
| Self-Determination |
Control of life decisions |
"Who defines the outcomes?" |
The distinction isn't academic hairsplitting. It shapes how states market programs, how families think about eligibility, how planners approach spending plan development, and yes—how technology vendors position themselves.
Why This Still Matters in 2026
The terminology split continues to influence program culture in subtle but meaningful ways.
Programs labeled "self-direction" tend to focus their messaging on budgets, compliance frameworks, and employer authority. The participant is positioned as a competent manager of services. Documentation emphasizes control, oversight, and accountability.
Programs labeled "self-determination" lean harder into choice, creativity, and non-traditional supports. The participant is positioned as the author of their own life story. Documentation emphasizes dreams, goals, and self-defined outcomes.
Both are valid. Both are necessary. And increasingly, providers operating across multiple states need to honor both mindsets simultaneously.
This is especially true as we see more innovation at the intersection of disability services and technology. AI in home care isn't about replacing human judgment—it's about clearing the path for better choices. Whether you call it self-direction or self-determination, the promise is the same: technology should expand autonomy, not constrain it.
The Quiet Bridge Between Two Worlds
Here's what you can say with absolute confidence: self-direction and self-determination are two lenses on the same promise.
One emphasizes how services are managed. The other emphasizes why they exist in the first place. Modern programs need both:
- The operational rigor that Medicaid requires
- The personal autonomy that participants deserve
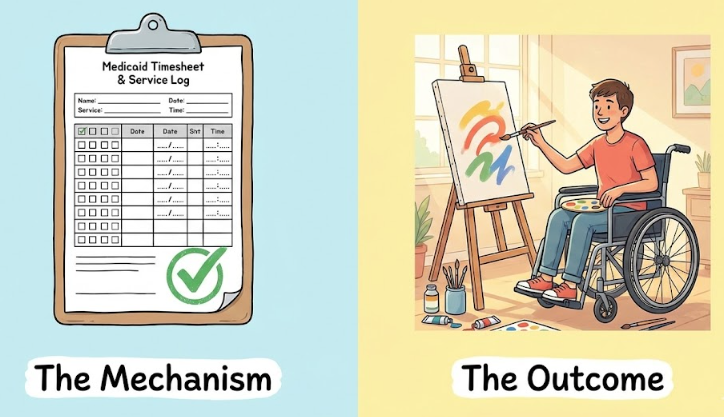
This is why comprehensive self-direction software can't just track budgets and timesheets. It needs to support the full spectrum of participant choice—from managing payroll for traditional caregivers to purchasing adaptive equipment, gym memberships, or cooking classes that build toward independence.
California's approach to spending plan flexibility, for example, has pushed other states to think more expansively about what "goods and services" can include. Meanwhile, the operational discipline that came from self-direction programs in other states has helped California maintain fiscal accountability as SDP scaled up.
The conversation flows both directions. Neither approach has a monopoly on wisdom.
What This Means for Your Program
If you're a provider, FMS agency, or state administrator, understanding this history helps you:
- Communicate more effectively with families. Some respond better to "you're in control of your services" language. Others connect more deeply with "you get to design your life" messaging. Know your audience.

- Build more flexible technology. A spending plan tool that works in California needs to accommodate creative, outcome-focused budget categories. A tool built for traditional self-direction states needs to accommodate employer authority workflows. Ideally, you build one platform that does both.
- Navigate multi-state operations smoothly. If you're operating in both California and non-California markets, you're already translating between these frameworks. Making the philosophical differences explicit helps your team stay consistent while adapting to local culture.
- Advocate for better policy. Understanding where both terms came from helps you argue for the best of both worlds: the operational clarity of self-direction combined with the expansive vision of self-determination.
The Promise Underneath the Words
Ultimately, whether you call it self-direction or self-determination, the core commitment is identical: people with disabilities should have the same freedom to shape their own lives that everyone else takes for granted.
The path to that promise ran through Medicaid waiver policy in most states. In California, it ran through disability rights organizing. Both were necessary. Both were right.
And both require technology, policy, and provider practice that honors what participants actually need: not just budget management tools, but systems that make genuine autonomy possible at scale.
That's the real work. The terminology is just the history we carry with us while we do it.
Best Self-Direction Software for FMS Agencies
Once you’re clear on the terminology, the next step is making sure your tech supports both models—our guide to the best self-direction software for FMS agencies walks through what that looks like in practice.
Ready to see how self-direction and self-determination come together in practice? Explore our comprehensive guide to self-direction programs, or see how our customizable spending plan tools adapt to California's unique requirements and beyond.
Ankota's mission is to enable the Heroes who keep older and disabled people living at home to focus on care because we take care of the tech. If you need software for home care, EVV, I/DD Services, Self-Direction FMS, Adult Day Care centers, or Caregiver Recruiting, please Contact Ankota. If you're ready to accept that the homecare agencies of the future will deliver care with a combination of people and tech, visit www.kota.care.
.png)
.png)



.png)
.png)


